Key Features And Benefits
Mobile Health (mHealth) apps are software programs designed to support healthcare and medical practice and run on smartphones, tablets, and other mobile devices. They can range from simple fitness trackers to sophisticated apps for the self-management of chronic diseases, for teleconsultations with doctors, and for retrieval of personal health records (PHRs). mHealth apps allow patients to take charge of their own health and health care by equipping them with tools for self-monitoring, communication with practitioners, and managing diseases anytime, anywhere. They are a significant part of the transformation of contemporary healthcare towards greater accessibility, individualization, and efficiency.
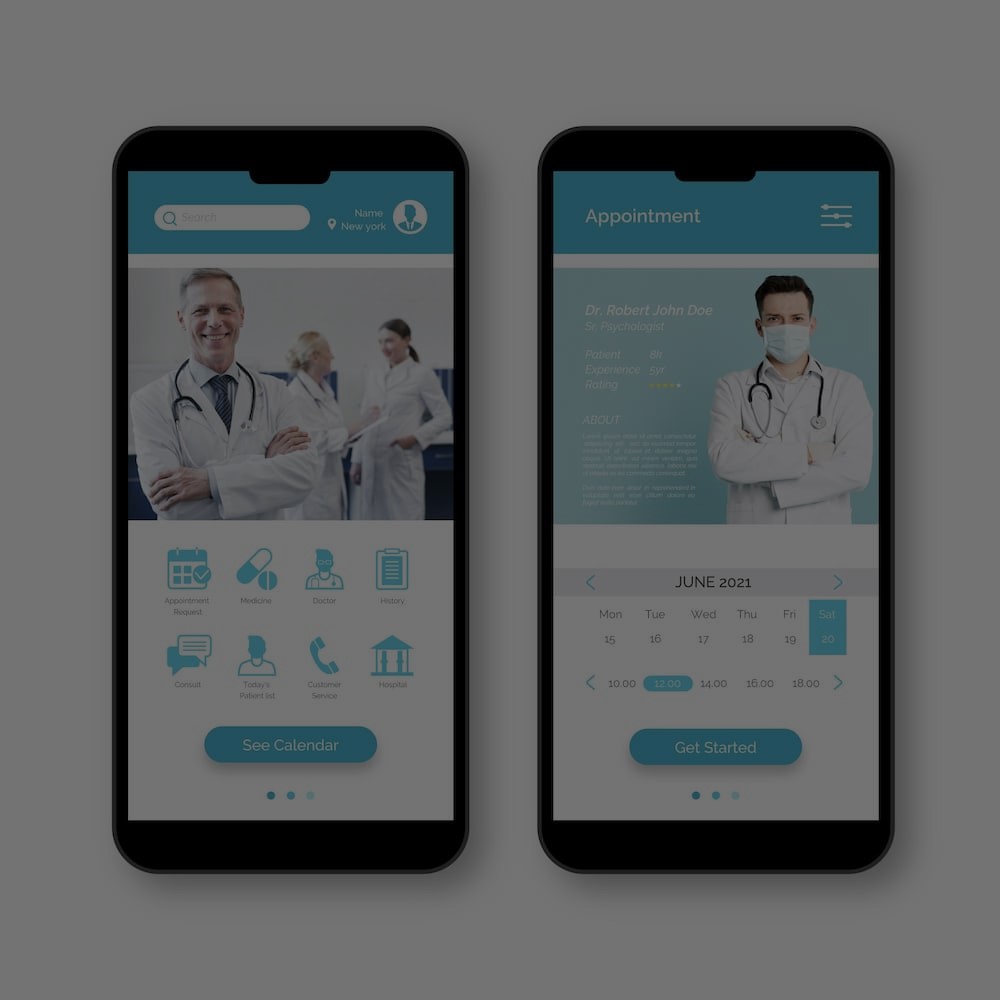
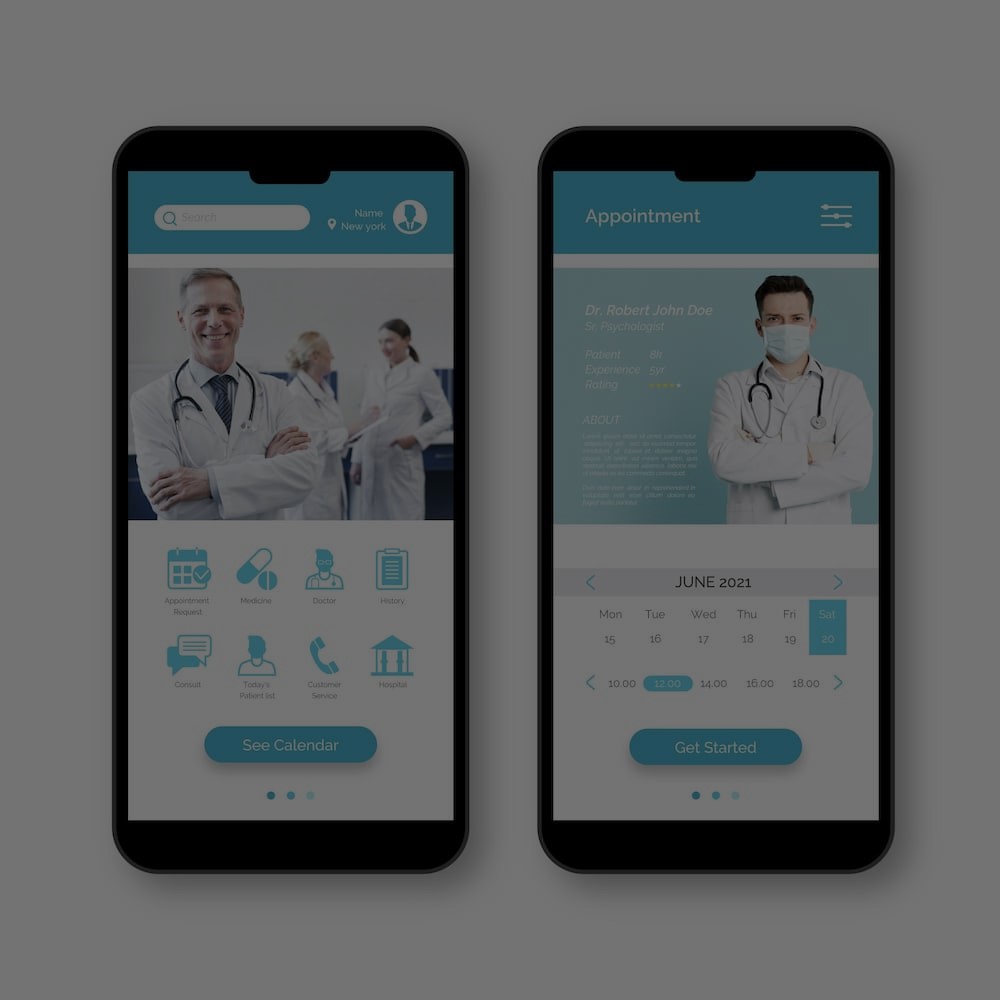
An appealing, user-friendly interface is essential to the enjoyment of any mHealth app. Intuitive charts and relatively uncomplicated and straightforward features help users interact with the app seamlessly, even if they are not technically skilled. A well-designed interface allows users to be involved without prolonged learning periods, increases the likelihood of frequent use, and enhances the engagement of patients. For healthcare professionals, an intuitive interface makes managing patient records and communicating with patients easier, thus saving time and opening discussions. Accessibility features, such as multiple languages, larger fonts, and support by a screen reader, likewise help influence a greater range of users.
One major concern in mHealth app development is security: the health data shared by a patient with an app may be deeply personal, so data must be well protected. Encryption of data, secure authentication of users, and perhaps inclusion of HIPAA (Health Insurance Portability and Accountability Act) awareness can ensure that your patient information is not shared with the highest stickler or hacker. Says Kusum, ‘Is it secure? That is an issue. You can change encryption, and you can add biometrics or a two-factor authentication code sent to your phone.’ by ensuring compliance with healthcare regulations for security and possible HIPAA compliance – your users will know they are working with a company dedicated to keeping their data safe and protected
Another feature that mHealth apps can possess is real-time health monitoring; patients can see their vital signs and fitness metrics or how well they are sticking to a treatment regimen. Real-time monitoring could be especially useful for patients with chronic health conditions such as diabetes or hypertension, where patients and physicians can remain alert for potentially dangerous occurrences over time. The benefits of routine monitoring are exemplified by the emergence of continuous glucose monitors that patients can wear to alert them about hypoglycemia (low blood sugar). Likewise, remote monitoring that not only tracks, but also forecasts safety-related mental health issues (eg, suicide risk), can provide support and care when and where it is needed. The possibility of monitoring and recording health metrics over time enables patients to play an active and engaged role in their health. It may yield valuable data to inform practitioner decision-making.
Personalization of mHealth apps helps in delivering personalized insights due to ongoing analysis of the user data to provide customized health insights like personalized health tips, feedback, and reminders that can help a user feel more involved in the health journey and be a customized health monitor. Examples of personalization include a mHealth app that may send users medical reminders based on when users last took their medication and what time the next dose is due. Personalization tends to increase user engagement, which, as a consequence, can help to improve health outcomes by monitoring health proactively.
MHealth apps also afford patients access to educational content, videos, and resources that increase health literacy, which can help them better engage in their own healthcare. This could include information about the condition itself and required care, along with the decision to pursue additional or complementary treatments. Educational content can also include information about lifestyle changes that may positively impact quality-of-life issues.
mHealth apps, by facilitating round-the-clock patient engagement, enhance direct contact with patients, which is one of the major complaints of both care providers and patients about the traditional healthcare system. With 24/7 access to physicians and health coaches via mobile apps, whether it’s a daily set of recommended health activities, tracking your steps, or transmitting vital signs, the real-time capabilities of mHealth Apps empower patients to be more involved in self-monitoring and proactive health maintenance, leading to better treatment adherence. By being more engaged, the approach to health care is perceived to be more patient-centric.
A significant advantage of mHealth apps lies in their ability to broaden the footprint and deepen the reach of healthcare services for geographically remote or underserved populations. By using digital access to healthcare resources, consultations, and monitoring tools, mHealth apps open up opportunities for healthcare services beyond the four walls of clinicians or hospital offices. Patients in rural areas can now consult specialists over videoconferencing tools instead of having to travel long distances for face-to-face visits and receive care remotely between appointments. The benefits of such enhanced access extend not only to healthcare outcomes in those populations but also indirectly to the health professional workforce, scaling up human resources in areas where they are most needed and contributing to greater equity in the fair distribution of healthcare provision.
mHealth apps also contribute to care coordination through improved communications and data-sharing between patients and health providers. Patients' health statuses can always be updated in real-time, enabling swift intervention and better decision-making. Regarding data-sharing, health providers can view and share data about the patient’s status across multiple platforms, such as test results, treatments, and progress, etc., helping other members of the care team to work together appropriately, minimizing errors, and ensuring the continuity of care and provision of the most effective treatment.
The influence of mHealth apps on patient health outcomes is direct and immediate, largely due to remote monitoring and timely intervention by both patients and clinicians. The real-time availability of personal health data generated by mHealth apps allows patients to track their health and function constantly and to obtain personalized feedback regarding trends in their health. This enables earlier diagnosis of potential disease, with consequent timely identification of intervention. For instance, an app that reports blood pressure can help a patient detect a concerning trend before the disease becomes extreme. Such early action leads to better disease management, reduced complications, and ultimately a healthier population, given that patients can remain actively engaged in tracking their health, thereby heading off serious issues.
Perhaps the greatest advantage of mHealth apps is the convenience and flexibility that they grant to patients in their ability to access healthcare on their own terms. Appointment scheduling, provider consultations and medication management are simplified by mHealth apps, easily accessible to patients at any time and in any location. Patients with erratic schedules, chronic conditions, or mobility problems will especially benefit from the flexibility of services delivered to their homes, their work, or any place they are able to access the internet from their communication devices. The convenience of mHealth apps enhances patient experiences by empowering patients’ control over their personal data and health status, facilitating continuity in care and thereby positively influencing health outcomes.
The biggest hurdle in developing mHealth apps is keeping them compliant with state regulations, such as the Health Insurance Portability and Accountability Act (HIPAA) in the US and the General Data Protection Regulation (GDPR) in the European Union. These and other regulations are meant to protect the privacy of users and provide security for sensitive medical information. Developers of mHealth apps must understand the regulatory framework in which their medical applications will be operating and build their apps to be compliant with these laws, most notably in the area of handling of data, storing sensitive medical information, and transmitting that information over networks.
Data security and privacy remain major concerns in mHealth app development due to its personal nature. Health information should be kept securely in the cloud while being safely transported to any desired recording device. App developers need to develop complicated yet uncompromised encryption protocols, secure authentication procedures, and access controls to try to protect such user data during transmission and storage. Lastly, the apps should also be designed to protect against other algorithms, vulnerabilities, and general insecurity issues, such as accidental data leakage and unauthorized leakages by hackers. Striking the sweet spot between security and usability remains a crucial part of mHealth app design because unless the security is implemented too simply, it can impede usability and discourage the adoption of apps. It would be great if the apps come with security patches and comply with emerging security standards in their implementation.
Another obstacle is to integrate the mHealth app with the wider healthcare IT infrastructure of the clinic – patient Electronic Health Records (EHRs), among others. Often, healthcare providers don’t use (or, heaven forbid, don’t have) a single system. Sometimes, systems come from different developers and may be technically incompatible with the new mHealth app. Seamless data integration across systems sounds like a no-brainer, but it’s technically difficult and can be time-consuming. The work involved requires careful planning, extensive testing, and sometimes even custom development. Being interoperable with other systems, using data standards, and ensuring that the mHealth app functions in multiple healthcare settings are just some of the hurdles to be overcome in order to develop an effective integrated application.
Even if a mHealth app is both well-designed and effective, the next challenge is to get users to adopt and continue using it. User adoption can be influenced by the app’s usability, perceived value, and context – that is, how easy it might be for the user to integrate the app’s use into their daily life. The challenge for the app developer, then, is to keep users more involved – for example, by offering periodic updates, promoting engagement, or providing regular reminders or feedback to encourage continued usage. A useful app is not enough. If users aren’t engaged, an app may not actually be useful. App design needs to be more than just functional. It has to be engaging. Users need to be able to experience a sense of agency when they use the app. This can mean they want to feel the app is a helpful and intelligent companion. Usage analytics can provide useful feedback on how to make the app more engaging, but it will take more work than simply including features like leaderboards, boss battles, or high scores. Understanding how the app is used and how that might change over time is crucial to iterative design and continuous development.
An Android app on illness self-management will fail to be useful for the range of people that it is intended for without a user-centered design approach. This requires the needs, preferences, and behaviors of the end-user (your end-user) to inform every stage of the process. A user-centric design helps boost not only user experience but adoption and retention rates – meaning that your app will actually remain a part of your user’s healthcare journey.
Security and compliance are foundational aspects of mHealth app development and are necessary to ensure the security of sensitive health data and regulatory compliance. Developers must ensure the app is designed to deliver on all relevant regulatory needs from the outset to achieve regulatory compliance. It isn’t good enough to apply a program set out by regulatory bodies like HIPAA in the US or GDPR (General Data Protection Regulation) in Europe as an afterthought. When these standards are an integral part of the design process for mHealth apps, they not only comply with legal needs but also enhance the security of user data. Once complied with, it’s important to keep up with evolving security threats and changes in regulations to maintain the whole process as we advance.
Flexibility means we build our app in a way that can satisfy the needs of our users as those needs change in the coming years. And they will change. Our healthcare practices will change over time. Technology will innovate. We cannot even imagine what new devices and apps will be available three years from now. Moreover, the ecosystem as a whole will grow – there will be more apps, more services, and more people using them. A scalable and flexible mHealth app will grow along with the ecosystem. It will not become outdated as the ecosystem does.
Users can help identify points of friction when navigating an app, point out unmet needs, and identify other opportunities to improve the app. By receiving regular feedback and incorporating it into an app over time, developers can keep it updated to meet people’s expectations of how the design evolves and how the app should work within relevant technological advancements over time. Some good practices include adding survey, rating, and in-app messaging functionalities to the app itself to allow direct feedback and conducting occasional user interviews or focus groups. By running a development process that embraces and wants to receive feedback, not only is the user experience improved, but also the loyalty that successful apps build over time.
To summarize, mHealth apps that are focused on key main features and benefits from user-centered design, robust data security, scalable, innovative features, and functions such as real-time monitoring and telemedicine can be of great value to increase medication adherence, improve health services access, and achieve better health outcomes. As the demand for digital health solutions continues to grow, the investment in well-designed, secure, and scalable mHealth apps will definitely shape the future path of the next century’s healthcare delivery.